 |
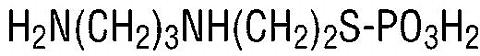
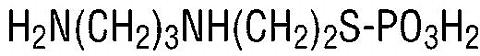
ETHYOL (amifostine) is an organic thiophosphate cytoprotective agent known chemically as 2-[(3-aminopropyl)amino]ethanethiol dihydrogen phosphate (ester) and has the following structural formula:
 |
Amifostine is a white crystalline powder which is freely soluble in water. Its empirical formula is C 5 H 15 N 2 O 3 PS and it has a molecular weight of 214.22.
ETHYOL is the trihydrate form of amifostine and is supplied as a sterile lyophilized powder requiring reconstitution for intravenous infusion. Each single-use 10 mL vial contains 500 mg of amifostine on the anhydrous basis.
ETHYOL is a prodrug that is dephosphorylated by alkaline phosphatase in tissues to a pharmacologically active free thiol metabolite. This metabolite is believed to be responsible for the reduction of the cumulative renal toxicity of cisplatin and for the reduction of the toxic effects of radiation on normal oral tissues. The ability of ETHYOL to differentially protect normal tissues is attributed to the higher capillary alkaline phosphatase activity, higher pH and better vascularity of normal tissues relative to tumor tissue, which results in a more rapid generation of the active thiol metabolite as well as a higher rate constant for uptake into cells. The higher concentration of the thiol metabolite in normal tissues is available to bind to, and thereby detoxify, reactive metabolites of cisplatin. This thiol metabolite can also scavenge reactive oxygen species generated by exposure to either cisplatin or radiation.
: Clinical pharmacokinetic studies show that ETHYOL is rapidly cleared from the plasma with a distribution half-life of <1 minute and an elimination half-life of approximately 8 minutes. Less than 10% of ETHYOL remains in the plasma 6 minutes after drug administration. ETHYOL is rapidly metabolized to an active free thiol metabolite. A disulfide metabolite is produced subsequently and is less active than the free thiol. After a 10-second bolus dose of 150 mg/m 2 of ETHYOL, renal excretion of the parent drug and its two metabolites was low during the hour following drug administration, averaging 0.69%, 2.64% and 2.22% of the administered dose for the parent, thiol and disulfide, respectively. Measurable levels of the free thiol metabolite have been found in bone marrow cells 5-8 minutes after intravenous infusion of ETHYOL. Pretreatment with dexamethasone or metoclopramide has no effect on ETHYOL pharmacokinetics.
Chemotherapy for Ovarian Cancer and Non-Small Cell Lung Cancer. A randomized controlled trial compared six cycles of cylophosphamide 1000 mg/m 2 , and cisplatin 100 mg/m 2 with or without ETHYOL pretreatment at 910 mg/m 2 , in two successive cohorts of 121 patients with advanced ovarian cancer. In both cohorts, after multiple cycles of chemotherapy, pretreatment with ETHYOL significantly reduced the cumulative renal toxicity associated with cisplatin as assessed by the proportion of patients who had >/=40% decrease in creatinine clearance from pretreatment values, protracted elevations in serum creatinine (>1.5 mg/dL), or severe hypomagnesemia. Subgroup analyses suggested that the effect of ETHYOL was present in patients who had received nephrotoxic antibiotics, or who had preexisting diabetes or hypertension (and thus may have been at increased risk for significant nephrotoxicity), as well as in patients who lacked these risks. Selected analyses of the effects of ETHYOL in reducing the cumulative renal toxicity of cisplatin in the randomized ovarian cancer study are provided in TABLES 1 and 2, below.
|
||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In the randomized ovarian cancer study, ETHYOL had no detectable effect on the antitumor efficacy of cisplatin-cyclophosphamide chemotherapy. Objective response rates (including pathologically confirmed complete remission rates), time to progression, and survival duration were all similar in the ETHYOL and control study groups. The table below summarizes the principal efficacy findings of the randomized ovarian cancer study.
|
||||||||||||||||||||||||||||||
A Phase II trial of ETHYOL, 740-910 mg/m 2 , and cisplatin, 120 mg/m 2 , administered on day 1 and vinblastine, 5mg/m 2 , administered on days 1, 8, 15 and 22 of each monthly cycle was conducted in 25 patients with Stage IV non-small cell lung cancer. This regimen was repeated until disease progression or unacceptable toxicity occurred, or a maximum of six cycles had been administered. Among 13 patients who received 4 or more cycles of this intensive cisplatin regimen, 1 had a >/=40% reduction in creatinine clearance. These results are consistent with the randomized ovarian cancer trial.
Sixteen of the 25 patients treated demonstrated a partial response to chemotherapy. With a median follow-up of 19 months, the median survival was 17 months. At one year, 64% of the patients were alive. These results indicate that ETHYOL may not adversely affect the efficacy of this chemotherapy for non-small cell lung cancer.
Radiotherapy for Head and Neck Cancer. A randomized controlled trial of standard fractionated radiation (1.8 Gy--2.0 Gy/day for 5 days/week for 5-7 weeks) with or without ETHYOL, administered at 200 mg/m 2 as a 3 minute i.v. infusion 15-30 minutes prior to each fraction of radiation, was conducted in 315 patients with head and neck cancer. Patients were required to have at least 75% of both parotid glands in the radiation field. The incidence of Grade 2 or higher acute (90 days or less from start of radiation) and late xerostomia (9-12 months following radiation) as assessed by RTOG Acute and Late Morbidity Scoring Criteria, was significantly reduced in patients receiving ETHYOL (TABLE 4).
|
||||||||||||||||
At one year following radiation, whole saliva collection following radiation showed that more patients given ETHYOL produced >0.1 gm of saliva (72% vs. 49%). In addition, the median saliva production at one year was higher in those patients who received ETHYOL (0.26 gm vs. 0.1 gm). Stimulated saliva collections did not show a difference between treatment arms. These improvements in saliva production were supported by the patients' subjective responses to a questionnaire regarding oral dryness.
In the randomized head and neck cancer study, locoregional control, disease-free survival and overall survival were all comparable in the two treatment groups after one year of follow-up (see TABLE 5).
|
||||||||||||||||||||||||||||||||||||
ETHYOL (amifostine) is indicated to reduce the cumulative renal toxicity associated with repeated administration of cisplatin in patients with advanced ovarian cancer or non-small cell lung cancer.
ETHYOL is indicated to reduce the incidence of moderate to severe xerostomia in patients undergoing post-operative radiation treatment for head and neck cancer, where the radiation port includes a substantial portion of the parotid glands (see Clinical Studies ).
For the approved indications, the clinical data do not suggest that the effectiveness of cisplatin based chemotherapy regimens or radiation therapy is altered by ETHYOL. There are at present only limited data on the effects of ETHYOL on the efficacy of chemotherapy or radiotherapy in other settings. ETHYOL should not be administered to patients in other settings where chemotherapy can produce a significant survival benefit or cure, or in patients receiving definitive radiotherapy, except in the context of a clinical study (see ).
ETHYOL is contraindicated in patients with known sensitivity to aminothiol compounds.
Patients should be adequately hydrated prior to the ETHYOL infusion and blood pressure should be monitored (see DOSAGE AND ADMINISTRATION ).
The safety of ETHYOL administration has not been established in elderly patients, or in patients with preexisting cardiovascular or cerebrovascular conditions such as ischemic heart disease, arrhythmias, congestive heart failure, or history of stroke or transient ischemic attacks. ETHYOL should be used with particular care in these and other patients in whom the common ETHYOL adverse effects of nausea/vomiting and hypotension may be more likely to have serious consequences.
Prior to chemotherapy, ETHYOL should be administered as a 15-minute infusion (see DOSAGE AND ADMINISTRATION ). Blood pressure should be monitored every 5 minutes during the infusion, and thereafter as clinically indicated.
Prior to radiation therapy, ETHYOL should be administered as a 3-minute infusion (see DOSAGE AND ADMINISTRATION ). Blood pressure should be monitored at least before and immediately after the infusion, and thereafter as clinically indicated.
Special consideration should be given to the administration of ETHYOL in patients receiving antihypertensive medications or other drugs that could cause or potentiate hypotension.
No long term animal studies have been performed to evaluate the carcinogenic potential of ETHYOL. ETHYOL was negative in the Ames test and in the mouse micronucleus test. The free thiol metabolite was positive in the Ames test with S9 microsomal fraction in the TA1535 Salmonella typhimurium strain and at the TK locus in the mouse L5178Y cell assay. The metabolite was negative in the mouse micronucleus test and negative for clastogenicity in human lymphocytes.
Pregnancy Category C. ETHYOL has been shown to be embryotoxic in rabbits at doses of 50 mg/kg, approximately sixty percent of the recommended dose in humans on a body surface area basis. There are no adequate and well-controlled studies in pregnant women. ETHYOL should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
No information is available on the excretion of ETHYOL or its metabolites into human milk. Because many drugs are excreted in human milk and because of the potential for adverse reactions in nursing infants, it is recommended that breast feeding be discontinued if the mother is treated with ETHYOL.
The safety and effectiveness in pediatric patients have not been established.
In the randomized study of patients with ovarian cancer given ETHYOL at a dose of 910 mg/m 2 prior to chemotherapy, transient hypotension was observed in 62% of patients treated. The mean time of onset was 14 minutes into the 15-minute period of ETHYOL infusion, and the mean duration was 6 minutes. In some cases, the infusion had to be prematurely terminated due to a more pronounced drop in systolic blood pressure. In general, the blood pressure returned to normal within 5-15 minutes. Fewer than 3% of patients discontinued ETHYOL due to blood pressure reductions. In the randomized study of patients with head and neck cancer given ETHYOL at a dose of 200 mg/m 2 prior to radiotherapy, hypotension was observed in 15% of patients treated.
Hypotension that requires interruption of the ETHYOL infusion should be treated with fluid infusion and postural management of the patient (supine or Trendelenburg position). If the blood pressure returns to normal within 5 minutes and the patient is asymptomatic, the infusion may be restarted, so that the full dose of ETHYOL can be administered.
Short term, reversible loss of consciousness has been reported rarely. Blood pressure reductions during ETHYOL administration have not been reported to cause long term CNS, cardiovascular or renal sequelae, but clinical studies performed to date have not evaluated the safety of ETHYOL in elderly patients or in patients with preexisting cardiovascular or cerebrovascular conditions.
Nausea and/or vomiting occur frequently after ETHYOL infusion and may be severe. In the ovarian cancer randomized study, the incidence of severe nausea/vomiting on day 1 of cyclophosphamide-cisplatin chemotherapy was 10% in patients who did not receive ETHYOL, and 19% in patients who did receive ETHYOL. In the randomized study of patients with head and neck cancer, the incidence of severe nausea/vomiting was 8% in patients who received ETHYOL and 1% in patients who did not receive ETHYOL.
Other effects which have been described during or following ETHYOL infusion are flushing/feeling of warmth, chills/feeling of coldness, fever, dizziness, somnolence, hiccups and sneezing. These effects have not generally precluded the completion of therapy.
Decrease in serum calcium concentrations is a known pharmacological effect of ETHYOL. At the recommended doses, clinically significant hypocalcemia has occurred rarely (<1%) (see ).
Allergic reactions have been reported with the use of ETHYOL. The majority of cases presented with the following symptoms: hypotension, fever, chills/rigors, dyspnea, skin rashes and urticaria. Other skin reactions including erythema multiforme, and in rare cases Stevens-Johnson Syndrome and toxic epidermal necrolysis, have been reported. There have been rare reports of anaphylactoid reactions including hypoxia, laryngeal edema, chest tightness, and possible cardiac arrest.
There have been rare reports of seizures in patients receiving ETHYOL.
TABLE 6 contains a summary of the more common adverse events from the two approved doses of ETHYOL:
|
|||||||||||||||||||||||||||||||||||||||||||||
In the randomized study of patients with head and neck cancer, 17% (26/150) discontinued ETHYOL due to adverse events. All but one of these patients continued to receive radiation treatment until completion.
In clinical trials, the maximum single dose of ETHYOL was 1300 mg/m 2 . No information is available on single doses higher than this in adults. In the setting of a clinical trial, pediatric patients have received single ETHYOL doses of up to 2700 mg/m 2 . At the higher doses, anxiety and reversible urinary retention occurred.
Administration of ETHYOL at 2 and 4 hours after the initial dose has not led to increased nausea and vomiting or hypotension. The most likely symptom of overdosage is hypotension, which should be managed by infusion of normal saline and other supportive measures, as clinically indicated.
For Reduction of Cumulative Renal Toxicity with Chemotherapy: The recommended starting dose of ETHYOL is 910 mg/m 2 administered once daily as a 15-minute i.v. infusion, starting 30 minutes prior to chemotherapy.
The 15-minute infusion is better tolerated than more extended infusions. Further reductions in infusion times for chemotherapy regimens have not been systematically investigated.
Patients should be adequately hydrated prior to ETHYOL infusion and kept in a supine position during the infusion. Blood pressure should be monitored every 5 minutes during the infusion, and thereafter as clinically indicated.
The infusion of ETHYOL should be interrupted if the systolic blood pressure decreases significantly from the baseline value as listed in the guideline below:
|
||||||||||||||||||
If the blood pressure returns to normal within 5 minutes and the patient is asymptomatic, the infusion may be restarted so that the full dose of ETHYOL may be administered. If the full dose of ETHYOL cannot be administered, the dose of ETHYOL for subsequent chemotherapy cycles should be 740 mg/m 2 .
It is recommended that antiemetic medication, including dexamethasone 20 mg i.v. and a serotonin 5HT 3 receptor antagonist, be administered prior to and in conjunction with ETHYOL. Additional antiemetics may be required based on the chemotherapy drugs administered.
For Reduction of Moderate to Severe Xerostomia from Radiation of the Head and Neck: The recommended dose of ETHYOL is 200 mg/m 2 administered once daily as a 3-minute i.v. infusion, starting 15-30 minutes prior to standard fraction radiation therapy (1.8-2.0 Gy).
Patients should be adequately hydrated prior to ETHYOL infusion. Blood pressure should be monitored at least before and immediately after the infusion, and thereafter as clinically indicated.
It is recommended that antiemetic medication be administered prior to and in conjunction with ETHYOL. Oral 5HT 3 receptor antagonists, alone or in combination with other antiemetics, have been used effectively in the radiotherapy setting.
ETHYOL (amifostine) for Injection is supplied as a sterile lyophilized powder requiring reconstitution for intravenous infusion. Each single-use vial contains 500 mg of amifostine on the anhydrous basis.
Prior to intravenous injection, ETHYOL is reconstituted with 9.7 mL of sterile 0.9% Sodium Chloride Injection, USP. The reconstituted solution (500 mg amifostine/10 mL) is chemically stable for up to 5 hours at room temperature (approximately 25°C) or up to 24 hours under refrigeration (2°C to 8°C).
ETHYOL prepared in polyvinylchloride (PVC) bags at concentrations ranging from 5 mg/mL to 40 mg/mL is chemically stable for up to 5 hours when stored at room temperature (approximately 25°C) or up to 24 hours when stored under refrigeration (2°C to 8°C).
CAUTION: Parenteral products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Do not use if cloudiness or precipitate is observed.
The compatibility of ETHYOL with solutions other than 0.9% Sodium Chloride for Injection, or Sodium Chloride solutions with other additives, has not been examined. The use of other solutions is not recommended.
ETHYOL (amifostine) for Injection is supplied as a sterile lyophilized powder in 10 mL single-use vials (NDC 17314-7253-1). Each single-use vial contains 500 mg of amifostine on the anhydrous basis. The vials are available packaged as follows:
3 pack--3 vials per carton (NDC 17314-7253-3)
Store the lyophilized dosage form at Controlled Room Temperature 20°-25°C (68°-77°F) [See USP].
U.S. Patents 5,424,471; 5,591,731
Manufactured by:
USB Pharma B.V.
6545 CG Nijmegen
The Netherlands
Or:
Ben Venue, Inc.
Bedford, Ohio 44146
Marketed by:
ALZA Pharmaceuticals
A division of ALZA Corporation
Palo Alto,
California 94303
And:
U.S. Bioscience, Inc.
West Conshohocken,
Pennsylvania 19428
1-800-506-4959
©1999, U.S. Bioscience, Inc.
Revision Date 6/99 N-LB2022 PE
 |